Standard automated perimetry not clinically useful for AMD: new publication
Perimetry is a fundamental part of assessing visual function in clinical practice, however clear evidence for its use in early age-related macular degeneration (AMD) is lacking.
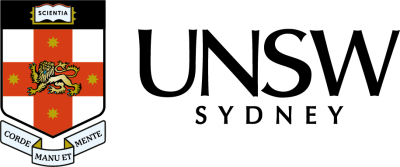
Dr Lisa Nivison-Smith and the research team at the Centre for Eye Health have recently completed a review of the literature and found while perimetry detects functional losses that are statistically significant in early and intermediate AMD, they are not clinically meaningful.
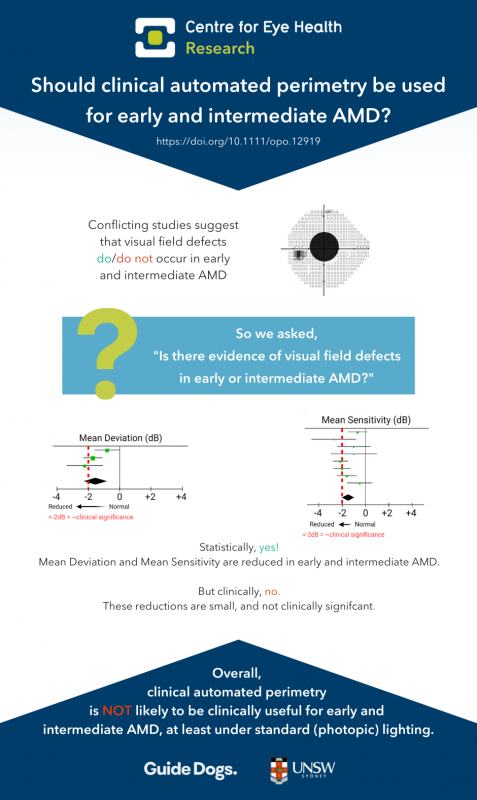
This means that standard automated perimetry under photopic conditions is unlikely to be useful for routine assessment of early AMD.
Age-related macular degeneration is a leading causes of irreversible blindness in developed countries with approximately one in seven Australians over 50 have signs of the disease.
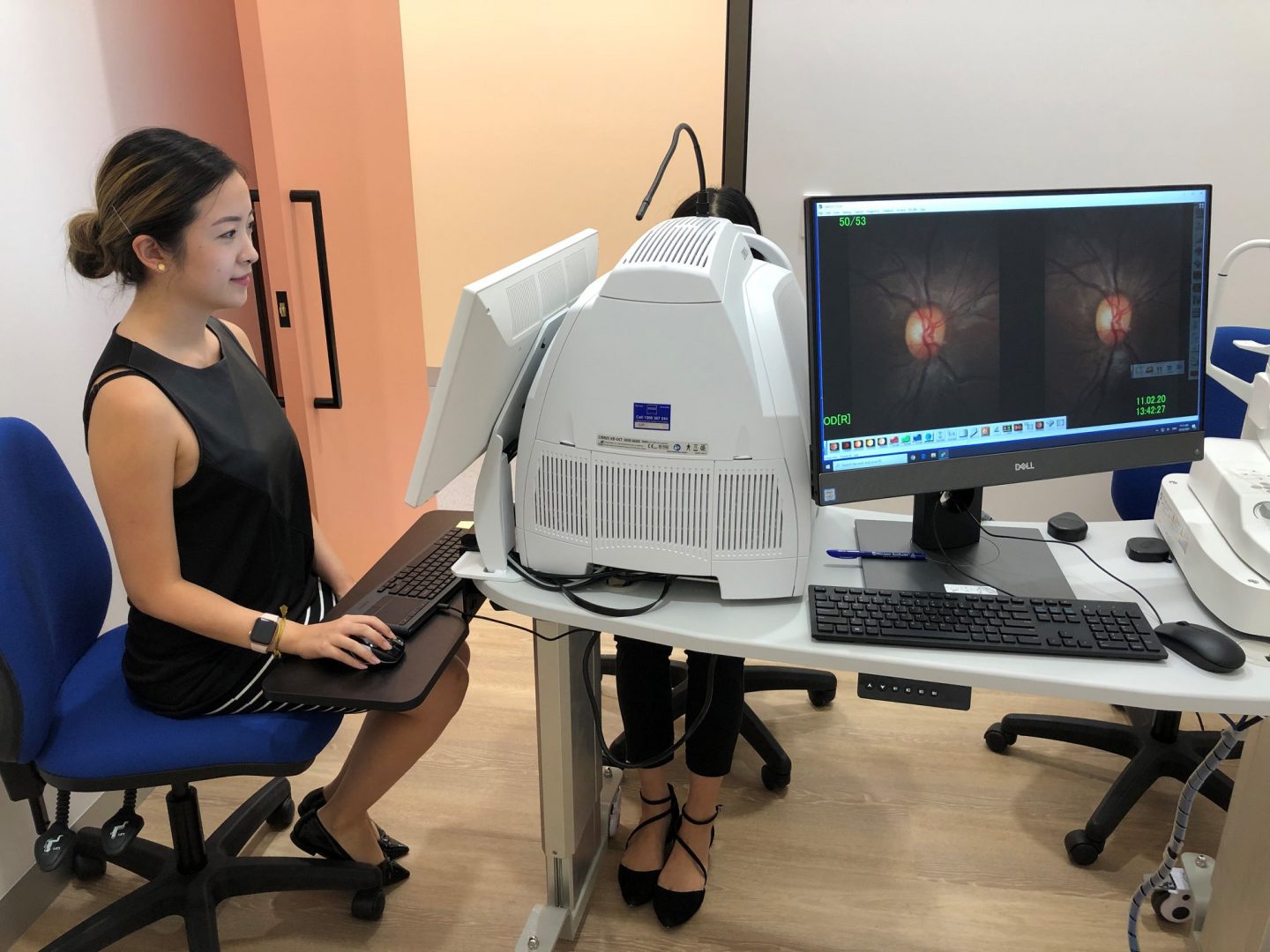
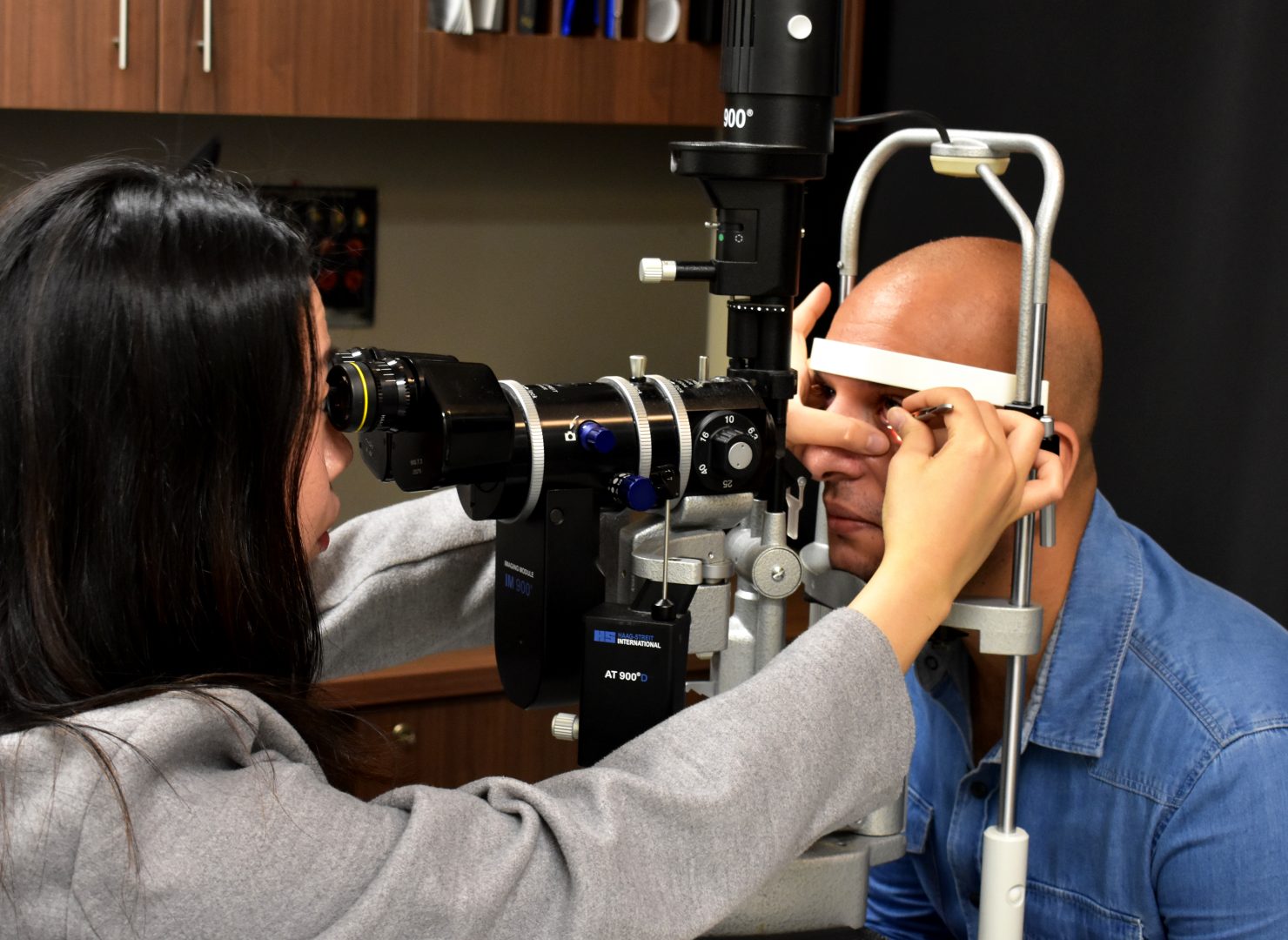
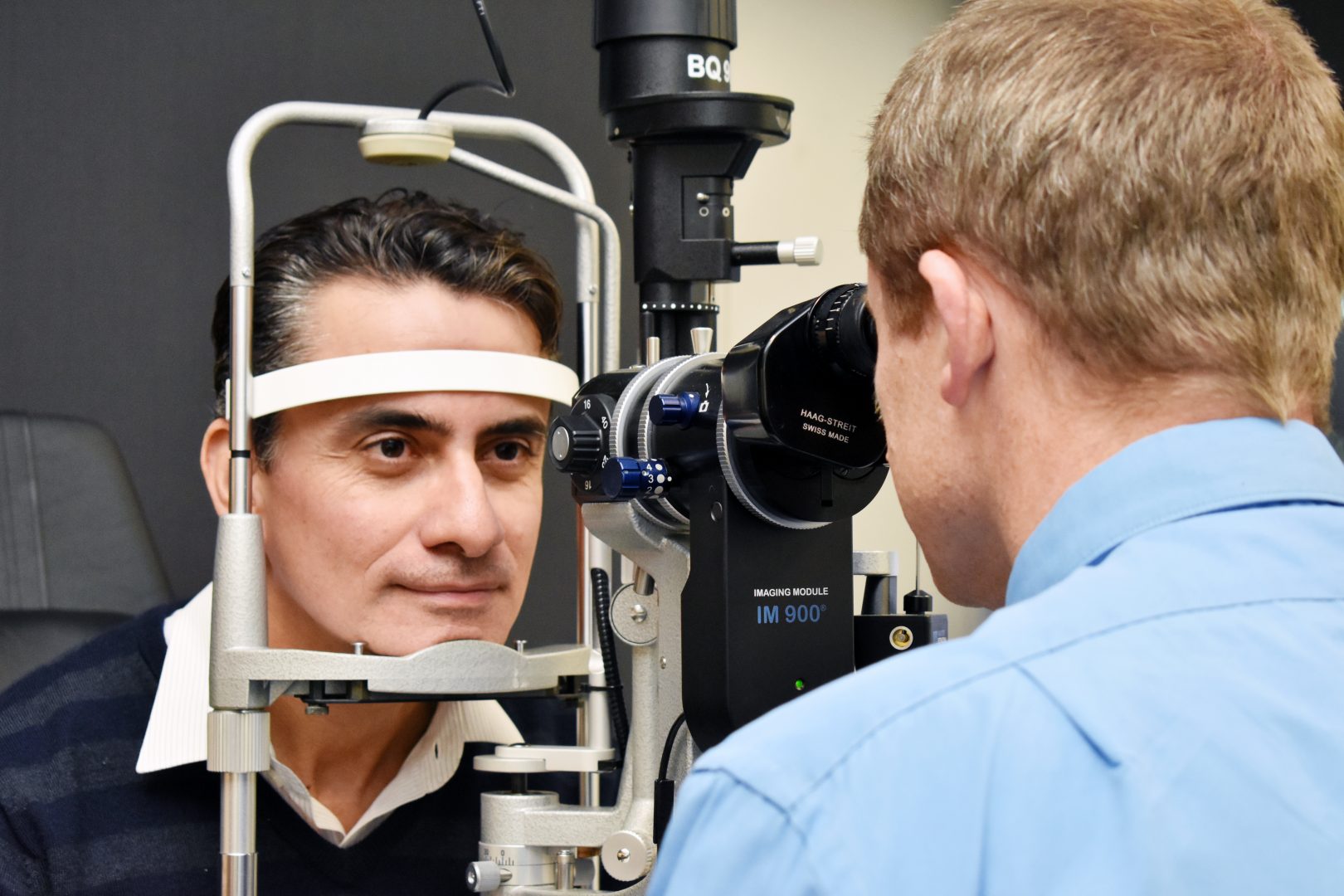
In Australia, optometric practice is at the forefront of AMD, typically detecting and diagnosing the early stages of disease. This is mostly through traditional and advanced ocular imaging technologies lead by various clinical guidelines. However, the role of functional testing in clinical assessment of early/intermediate AMD, particularly using perimetry, is less clear. A literature search of perimetry and AMD will yield thousands of results, many suggesting differences in various visual field measures using various forms of perimetry in association with disease. Yet in current clinical practice, anecdotally, standard automated perimetry is not generally performed for individuals with early or intermediate AMD.
We addressed this gap by asking the question – should clinical automated perimetry be considered for routine functional assessment of early/intermediate AMD?
To answer this, we reviewed studies that used what they defined as “clinically available perimetry” to assess AMD. These were commercially accessible, non-modified automated perimetry devices and protocols used in current clinical practice such as standard (white-on-white) automated perimetry, flicker perimetry, and frequency-doubling technology. This inclusion criteria were chosen to emphasise the clinical relevance of the results.
After reviewing 26 papers, we found significant reductions in global and local visual field indices for early and intermediate AMD eyes compared to normal eyes. However, despite large statistical effect sizes, these reductions were not clinically meaningful. We also found limited evidence on links between visual field and real-world patient outcomes.
These results suggest clinically available perimetry in routine assessment of the early stages of AMD is likely not useful. However future work using perimetry under non-standard conditions may warrant further investigation.